26 January 2026
Walking is far more than a physical act; it is a complex reflection of our respiratory, neurological, and psychological health.
While standard clinical evaluations remain essential for diagnosis, there is a growing recognition of the need to complement these “point-in-time” assessments with long-term data collected in a patient’s natural environment. In this context, gait speed (GS) has emerged as the “sixth vital sign” offering a sensitive and reliable metric for predicting health outcomes across different conditions, such as cardiovascular, respiratory, neurodegenerative and psychiatric diseases.
In patients with chronic obstructive pulmonary disease (COPD), mobility loss is a primary prognostic factor for mortality and increased healthcare costs. However, despite its significance, real-world mobility tracking is not yet a standard clinical practice. Bridging this gap through non-invasive sensors and AI-driven predictive algorithms is crucial for improving disease management, identifying exacerbations early and personalizing long-term patient care.
TOLIFE solution: a multimodal approach to personalized care
To address the clinical imperative for a longitudinal mobility surveillance in COPD patients, the European Union-funded TOLIFE project has developed a pioneering methodology designed to bring diagnostic precision into the patient’s home. By using Artificial Intelligence and discreet sensors that monitor heath conditions during daily life activities, TOLIFE aim to predict flare-ups and to provide personalized interventions, ultimately improving the quality of life for COPD patients.
As a central part of this mission, TOLIFE has conducted a scientific study to develop a novel method for estimating gait speed from a heterogeneous set of wearable devices. The research investigated how smartphones, smartwatches and smart shoes can work both independently and in concert to provide accurate mobility insights: by exploring these technological synergies, TOLIFE developed a flexible framework that adapts to each patient’s lifestyle, allowing them to use whichever combination of devices they find most comfortable or accessible.
From wrist to feet: How AI decodes every step
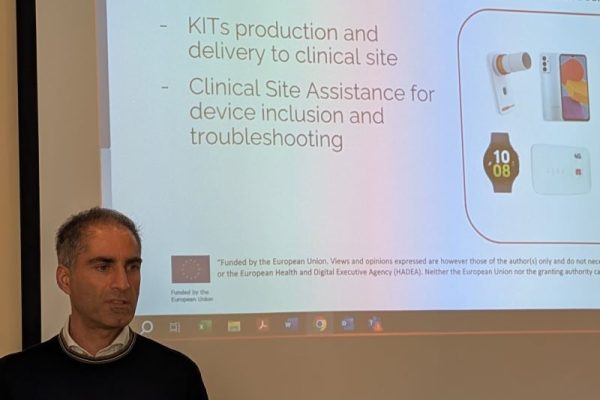
This specific study focused on three daily items from the TOLIFE kit:
- a smartphone;
- a smartwatch;
- a pair of smart shoes.
The smartwatch and the smartphone use internal motion sensors to track the patient’s balance and movement patterns. The smart shoes have an electronic unit integrated into the heel area of the insole and three pressure sensors that monitor how the foot strikes the ground. TOLIFE team built two specialized Android apps to gather information from the phone and watch sensors. The smartphone app also functioned as a hub to receive data from the smart shoes via Bluetooth. By bringing together data from the wrist, the pocket and the feet, the system creates a complete picture of a patient’s mobility.
To verify the model’s accuracy, the data sensors were compared with that of a high-precision professional system, called Xsens Awinda. This system makes use of 17 sensors placed across the body to measure movement speed with extreme precision. The data collected by this reference system have been used as benchmark to train our model to correctlymeasure walking speed.
The research involved 20 young healthy volunteers who wore the reference system and the experimental devices, with the smartwatch on the left wrist and the smartphone in the front pocket.
The subjects had to perform a modified version of the of the Six-Minute-Walking-Test (6MWT), which required them to walk along a 10-meter flat path, allowing about 50 cm for each turn. Each person completed the test three times at different speeds: slow, medium and fast; this allowed to analyze how the sensors recorded movement across a wide range of walking paces while keeping the devices in the same position.
To find the most accurate setup for tracking movement in daily life, the devices were employed one by one, collectively or in combination. Therefore, 7 different systems were tested:
- phone;
- watch;
- shoes;
- phone + watch;
- phone + shoes;
- watch + shoes;
- all the devices.
The study evaluated the accuracy of every configuration of wearable sensors, identifying the key variables that most heavily influence the AI-driven predictive models.
Therefore, 7 distinct machine learning models were created, one for every possible combination of these devices: after a pre-processing phase of the raw data, the sensor signals were divided into small 5-second segments; from these segments, several key statistical values (features) were extracted (148 for phone and watch, and 222 for shoes), so a smart selection process was applied to isolate only the 10 most important characteristics for each device combination. After defining the models’ mathematical formulas, the algorithm was validated through the “Leave-One-Subject-Out”approach: the model was trained on data from all subjects, excluding one individual used as a final test case; this procedure was repeated for each participant to ensure the system is robust and functions correctly with any new user.
Which wearable combination truly wins?
The findings demonstrated that the models achieved a high level of accuracy in estimating walking speed.

The standalone contenders
At first glance, the smartphone appears to be the champion of accuracy. Because it’s typically carried in a pocket, close to the body’s center of mass, it provides very precise speed readings. However, during the tests, the phone was kept in a fixed controlled position. In real life, phones bounce around or sit in bags, which might make these results hard to replicate.
In contrast, the smartwatch proved to be a more reliable “all-rounder”. While it may be slightly less accurate than the phone on its own, its consistent presence on the wrist ensures more dependable data in real-world conditions. Furthermore, the smartwatch captures additional physiological metrics, such as heart rate (HR), which could potentially further enhance prediction accuracy.
The winning combination
The real breakthrough occurred through the pairing of multiple devices. It was found that the ultimate “effective formula” for tracking walking is the smartwatch paired with smart shoes. This duo achieved the highest level of accuracy, outperforming even the most stable smartphone readings. It appears that data from the wrist and the feet complement each other, effectively filling the information gaps that a single device might miss.
The surprise: less is more
Interestingly, evidence suggests that using all devices at once actually worsened the results. This might seem counterintuitive, but it is primarily due to “data noise”. When a model receives too much overlapping information from various sensors, it struggles to distinguish between relevant and redundant data, which in turn reduces its predictive power.
Future perspectives: A new era of flexible health monitoring
This research marks a significant milestone in wearable technology, showcasing how a strategic assembly of devices can redefine health monitoring in real-world settings. By moving beyond the reliance on a single sensor, TOLIFE system utilizes an intelligent algorithm that adapts to any combination of these three tools. This creates a robust failsafe: whether the devices work together as a powerhouse ensemble for maximum precision or function independently, the flow of health data remains uninterrupted and accurate, even if one device runs out of power or is temporarily removed.
The true value of this multi-device approach lies in its patient-centered design. Giving individuals the flexibility to choose the most suitable device for their daily activities significantly improves long-term compliance. For those managing chronic conditions like COPD, this means moving from reactive to proactive care. By detecting subtle, day-to-day changes in mobility, clinicians can personalize treatment plans and intervene early, potentially preventing complications and enhancing overall quality of life.
Ultimately, this framework offers a new standard for remote healthcare. While particularly effective for respiratoryhealth, its implications extend to any condition where mobility is a key indicator, such as Parkinson’s disease, heart failure or mental disorders. This study proves that the future of medical monitoring lies in technology that is as dynamic and adaptable as the patients who use it.
Interested to know more about this research? Read the full scientific article here: https://www.mdpi.com/1424-8220/24/10/3205